Dental health is an essential aspect of our overall well-being, and any issues concerning our teeth and gums should not be taken lightly. One such problem that individuals may encounter is inflammation of the dental nerve, also known as pulpitis. Pulpitis can cause severe discomfort and pain, making it crucial to understand its causes, symptoms, and diagnosis. In this article, we will explore the various aspects of pulpitis, including effective treatment options, and prevention and self-care tips to manage dental nerve inflammation. By gaining a comprehensive understanding of pulpitis, individuals can take proactive measures to maintain optimal dental health and prevent further complications.
1. Understanding Pulpitis: Causes, Symptoms, and Diagnosis
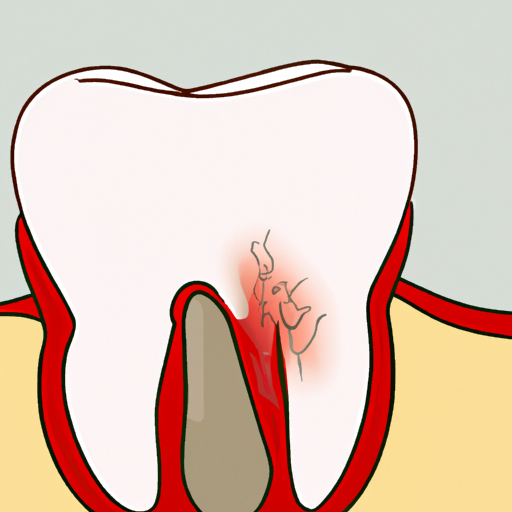
Pulpitis refers to the inflammation of the dental nerve, also known as the dental pulp. It is a common condition that can cause significant discomfort and pain. Understanding the causes, symptoms, and diagnosis of pulpitis is essential for effective treatment and management.
Causes:
Pulpitis can occur due to several factors, with the most common cause being dental decay. When a cavity forms in the tooth, bacteria can penetrate the enamel and dentin layers, reaching the pulp and causing an infection. Trauma to the tooth, such as a fracture or injury, can also lead to pulpitis. Additionally, repetitive dental procedures or extensive dental work can irritate the pulp, leading to inflammation.
Symptoms:
The symptoms of pulpitis can vary in severity, depending on the extent of inflammation and individual pain tolerance. Common symptoms include persistent toothache, especially when biting or chewing. The pain may be sharp or throbbing and can radiate to the jaw, ear, or head. Increased sensitivity to hot or cold temperatures is another symptom of pulpitis. In some cases, individuals may experience swelling around the affected tooth, bad breath, or a foul taste in the mouth.
Diagnosis:
Diagnosing pulpitis involves a thorough examination by a dental professional. The dentist will inquire about the patient's symptoms and medical history, paying particular attention to any recent dental procedures or trauma. A visual examination of the affected tooth will be conducted, looking for signs of decay or
2. Effective Treatment Options for Dental Pulpitis
Effective Treatment Options for Dental Pulpitis
When it comes to the treatment of dental pulpitis, the primary goal is to alleviate pain and preserve the health of the affected tooth. The treatment options for this condition may vary depending on the severity of inflammation and the stage of pulpitis. Here are some effective treatment options commonly used by dental professionals:
1. Medications: In cases of mild to moderate pulpitis, dentists often prescribe nonsteroidal anti-inflammatory drugs (NSAIDs) to reduce pain and inflammation. Over-the-counter pain relievers such as ibuprofen or aspirin may also be recommended. These medications can provide temporary relief and help manage the symptoms until further treatment is initiated.
2. Pulpotomy: This procedure involves the removal of the infected or inflamed portion of the dental pulp. It is typically performed on primary teeth or young permanent teeth. After removing the affected pulp, the dentist applies a medicated dressing to promote healing. This technique is effective in preserving the vitality of the remaining healthy pulp.
3. Root Canal Therapy: Root canal treatment is often necessary for cases of severe pulpitis or when pulpitis progresses to irreversible pulpitis. During this procedure, the infected pulp is completely removed, and the root canal system is thoroughly cleaned and disinfected. The canals are then filled with a biocompatible material to seal off any potential reinfection. A dental crown may be placed over the treated tooth to restore its strength
3. Prevention and Self-care Tips to Manage Dental Nerve Inflammation
Prevention and Self-care Tips to Manage Dental Nerve Inflammation
While dental nerve inflammation, also known as pulpitis, can be a painful and uncomfortable condition, there are steps you can take to prevent it and manage the symptoms. By adopting good oral hygiene practices and making a few lifestyle changes, you can significantly reduce the risk of developing pulpitis and maintain a healthy dental nerve. Here are some prevention and self-care tips to keep in mind:
1. Maintain Proper Oral Hygiene:
One of the most effective ways to prevent dental nerve inflammation is by practicing good oral hygiene. Brush your teeth at least twice a day using a fluoride toothpaste and a soft-bristled toothbrush. Pay attention to all areas of your mouth, including the back teeth and along the gumline. Additionally, flossing daily helps remove plaque and food particles from between your teeth, preventing any potential dental infections.
2. Regular Dental Check-ups:
Regular dental check-ups are essential in preventing and managing dental nerve inflammation. Dentists can identify early signs of tooth decay, gum disease, or any other oral health issues that could lead to pulpitis. By addressing these problems promptly, you can prevent the inflammation of the dental nerve and potential complications. Aim for dental visits every six months or as recommended by your dentist.
3. Avoid Triggering Factors:
Certain habits and lifestyle choices can increase the risk of dental nerve inflammation. Avoid excessive consumption of sugary and acidic foods and